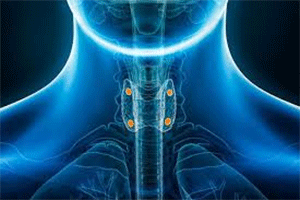
What Are Parathyroid Glands?
The parathyroid glands, (highlighted in the image above in yellow), are in the neck behind the butterfly-shaped thyroid gland. Despite their very small size, (each one is typically the size of a grain of rice), their role is to continuously monitor and closely regulate the calcium in our bodies to keep it within a very narrow range – between 8.5 and 10.2 mg/dL.
What the Parathyroid Glands Do for Our Bones
Our bodies are in a constant state of “bone remodeling,” where old bone tissue is broken down and new bone tissue is formed. This process relies heavily on calcium. The parathyroid glands, sometimes referred to as the “calcium thermostat”, help control the body’s calcium balance by producing parathyroid hormone (PTH). Here’s how that works:
Low calcium (hypocalcemia): When blood calcium levels drop, the parathyroid glands release more PTH which signals the bones to release calcium into the bloodstream. At the same time, they signal the kidneys to excrete less calcium in the urine and the digestive tract to absorb more calcium.
High calcium (hypercalcemia): When blood calcium levels are too high, the glands reduce PTH production, allowing blood calcium levels to return to a normal range.
The Danger of Overactive Parathyroid Glands
When one or more parathyroid glands become overactive, it is a condition called primary hyperparathyroidism (PHPT). Secondary hyperparathyroidism is a response to another underlying condition, such as chronic kidney disease, that causes low blood calcium and triggers the parathyroid glands to produce more PTH to correct it.
While most cases of osteoporosis are caused by normal aging, another leading cause is primary hyperparathyroidism. This usually occurs due to a non-cancerous growth on the gland called an adenoma, which causes overproduction of PTH. This excessive PTH, (which can be measured in a blood test), causes the bones to release calcium into the bloodstream, weakening the bones in the process.
About 90% of the time, only one gland is affected. Less commonly, two parathyroids develop adenomas. (More than two is very uncommon.) For most people, it is routine bloodwork that catches hypercalcemia caused by PHPT. However, it’s possible that unexplained symptoms such as ongoing fatigue, bone, joint, or muscle pain, memory issues or difficulty concentrating, increased thirst or more frequent urination, and depression or anxiety are caused by PHPT.
While it’s important to note that these symptoms can be caused by many other things, when they are related to PHPT, it’s directly related to the length of time your blood calcium levels stay above the normal range. The longer hypercalcemia goes untreated, the more likely it is that some of these symptoms occur.
Tests for Primary Hyperparathyroidism
If your healthcare provider suspects that you have PHPT, some of the tests that may be performed include:
Blood tests – If a blood test shows that you have hypercalcemia, the test will likely be repeated because other conditions can raise the level of calcium in the blood, so a closer look is warranted. PTHP can be diagnosed if blood tests also show that you have a high level of parathyroid hormone.
Bone mineral density test (DXA scan) – People with PHPT may not have any signs other than low bone density as measured on a DXA scan. Interestingly, bone loss is predominantly seen when the forearm is scanned, because of the type of bone cells that are prevalent there.
Urine test – Testing a sample of urine collected over 24 hours can show how well the kidneys are working and how much calcium is in the urine. The test also can help determine if a kidney problem is causing hyperparathyroidism.
Surgery is the Only Definitive Cure for Primary Hyperparathyroidism
All people, regardless of age, with PHPT will eventually get osteoporosis if the parathyroid adenoma is not removed (1). If you are diagnosed with PHPT, the most common and effective treatment is surgery to remove the overactive gland. This low-risk procedure can lead to a dramatic improvement in bone density over time and can actually reverse the osteoporosis caused by this condition.
If surgery is recommended, imaging tests will be performed to locate the parathyroid gland(s) that are affected. This may be a Sestamibi parathyroid scan which uses a radioactive substance taken up by parathyroid glands when they make too much parathyroid hormone.
Primary Hyperparathyroidism is Often Underdiagnosed
PHPT is the leading cause of hypercalcemia and secondary osteoporosis*, yet it is often both underdiagnosed and undertreated. Balentine and colleagues looked at the records of over 10,000 patients with hypercalcemia and found that only 32% had their PTH levels measured to determine the underlying cause (2).
Dawood and colleagues found that of 3151 patients with persistent hypercalcemia, only 48% had their PTH measured (3):
“Within a large academic health system, more than half of patients with confirmed hypercalcemia were not assessed for PHPT, including many patients with pre-existing bone disease.
Care gaps in bone mineral density assessment and medical or surgical therapy represent missed opportunities to avoid skeletal and other complications of PHPT.”
In Summary
If you have osteoporosis, be aware of the role your parathyroid glands may be playing in undermining your effort to keep your bones strong. If you or your doctor have any reason to suspect a parathyroid issue, checking your PTH and calcium levels is a simple and vital step toward strengthening your bones.
Always consider getting another opinion. In all things, each of us must be our own healthcare advocate.
*Secondary osteoporosis is a type of osteoporosis that occurs because of something other than the aging process, such as a specific underlying medical condition or medication.
- Bilezikian JP, et al. Management of Primary Hyperparathyroidism. Journal of Bone and Mineral Research 2022;37(11):2391-2403. doi:10.1002/jbmr.4682
- Balentine CJ, et al. Failure to Diagnose Hyperparathyroidism in 10,432 Patients with Hypercalcemia: Opportunities for System-level Intervention to Increase Surgical Referrals and Cure. Annals of Surgery 2017 Oct;266(4):632-640. doi: 10.1097/SLA.0000000000002370
- Dawood NB, et al. Systems-Level Opportunities in the Management of Primary Hyperparathyroidism: An Informatics-based Assessment. Journal of Clinical Endocrinology and Metabolism 2021;106(12):e4993-e5000. doi:10.1210/clinem/dgab540
Additional reading:
The website www.parathyroid.com has a wealth of clearly presented information on this topic and I recommend it despite the underlying heavy marketing of their own program.